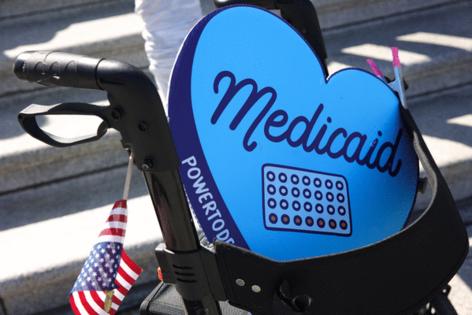
Medicaid cuts could be dangerous for cancer survivors
Published in News & Features
When Valerie Brown’s lung cancer returned and began to spread to other parts of her body, her doctors suggested a drug that would slow the cancer’s growth.
She’d already had surgery and radiation, and eliminating the cancer was no longer an option. Most people with her type of cancer live no more than five years.
Six years later, the 62-year-old South Jersey woman is enjoying watching her 10 grandchildren grow up. She credits Tagrisso, a drug designed to treat her specific form of cancer. It costs about $18,000 a month and has been covered by her Medicaid plan.
But Brown fears she could soon lose access to the drug.
Earlier this year, the Trump administration approved $900 billion in sweeping cuts to Medicaid, the publicly funded health program for low-income families and people with disabilities. Democrats are now demanding that Republicans address some of their concerns about patients who rely on safety-net healthcare programs, which has led to a deadlock in Washington over a federal spending plan and the ongoing government shutdown.
The law requires people to provide monthly proof of employment and renew their plan every six months are expected to leave millions uninsured in the coming years, including 300,000 in Pennsylvania and 350,000 in New Jersey.
Brown, who is eligible for Medicaid because of a disability, worries that she could lose her plan, or that the massive funding cuts could lead states to change how their Medicaid plans cover expensive drugs like Tagrisso.
“I’d be facing my mortality,” said Brown, who was diagnosed at age 49, without a history of smoking.
The pending Medicaid cuts could have particularly dangerous and costly implications for cancer care, researchers and advocacy groups warn. People who rely on Medicaid to pay for cancer treatment and ongoing monitoring are less likely to be able to meet the work requirements needed to keep their plan because of their poor health.
Losing coverage may also mean fewer people get routine screenings, such as mammograms and colonoscopies, which are key to identifying breast and colon cancer early, when it is easier and less costly to treat. This could mean more cancers diagnosed at later stages, at greater financial cost to patients and taxpayers, who foot a portion of the bill for Medicaid.
“When cancer is detected later, it has an effect on our whole system,” said Ann Nguyen, an associate research professor and scientist at the Rutgers Center for State Health Policy. “It’s going to be an increasingly difficult environment to navigate.”
Targeted for Medicaid cuts
Brown does not know exactly what the Medicaid cuts approved by the Republican-led Congress this summer will mean for her care.
Their primary target is lower-income, working adults who gained access to Medicaid through the 2010 Affordable Care Act. The so-called Obamacare law allowed states to expand access that had previously been restricted to families with children, pregnant people, and individuals with disabilities.
Just under 2 million New Jersey residents are covered by Medicaid, and about 680,000 are eligible because of expansion rules, according to the most recent data from the Centers for Medicare and Medicaid Services.
In Pennsylvania, about 750,000 of the 3 million people covered by Medicaid fall within the expansion group, according to the Pennsylvania Department of Human Services.
People who qualify under Medicaid expansion have incomes below 138% of the federal poverty rate — an annual income of about $21,500 for an individual. Previously, many earned too much to qualify for Medicaid, but were largely in jobs that did not offer health insurance, leaving them uninsured.
Nguyen and her colleagues at Rutgers say cutting Medicaid will mean more people are once again without health insurance to cover the routine screenings that help detect cancer early.
States that expanded Medicaid access saw more than 2,500 early cancer diagnoses within the first five years of the new law, saving millions in taxpayer spending, according to the American Cancer Society. Early diagnosis is critical because late-stage cancers can cost up to seven times more to treat, according to the national nonprofit.
Late-stage treatment can be especially hard on patients because they are less likely to have jobs with paid leave benefits. Taking time off for cancer treatment could mean going without pay or losing their job, Nguyen said.
In Washington, Democrats have pointed to patients like Brown, who rely on safety-net healthcare programs to afford ongoing care, in their opposition to the Medicaid cuts.
Their demands in the current budget impasse are centered on extending tax credits, due to expire at the end of the year, that help many working adults afford Obamacare health plans. Republicans have blamed the government shutdown on Democrats’ unwillingness to budge on healthcare demands.
A New Jersey woman’s cancer journey
Brown was just a year shy of her 50th birthday and had been struggling with breathing problems for months when a specialist sent her for a CT scan and found cancer in her left lung.
There was little Brown could have done to catch the cancer early, since screening tests are typically recommended for people over age 50 with a history of smoking.
Brown had never been a smoker, and did not have a family history of lung cancer.
Brown had surgery and radiation, but the cancer showed up again on a monitoring scan years later, this time in her right lung and lymph nodes.
Cancer is much harder to treat once it has metastasized, or spread to other organs.
Her care was covered by her Medicaid plan. Years later, when her cancer returned, Medicaid also covered Tagrisso, which is designed to help slow the growth of Brown’s specific type of lung cancer.
Without Medicaid, she would not be able to afford the drug and would have to stop taking it.
Under the new rules, people who qualify for Medicaid because of a disability are exempt from the work requirements. But Brown is still fearful she could lose her plan or that changes to prescription drug cost-sharing could make her medication unaffordable.
It is unclear what people who are exempt from work requirements will need to do to prove their disability status. Analysts have pointed to prescription drug coverage as one of the service areas that states may scale back as they look to balance the massive federal cuts in their Medicaid budgets.
Brown’s voice cracks as she talks about the possibility, because she has so much more to do, she says.
She has been a volunteer with the American Cancer Society for years, and makes frequent trips to visit her grandchildren, who range in age from 4 to 17, grow up.
“I am hoping to be around for a long time,” she said, “to see all my little ones graduate and fulfill their dreams.”
©2025 The Philadelphia Inquirer, LLC. Visit at inquirer.com. Distributed by Tribune Content Agency, LLC.


Comments