Commentary: Early cancer detection, with new tools and genetic testing, saves lives
Published in Op Eds
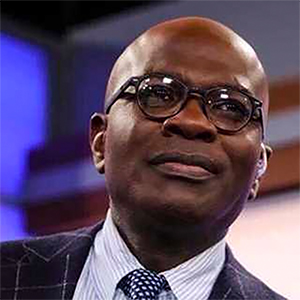
After surviving three types of cancer and having to face the harsh realities of colorectal and endometrial cancer and basal cell carcinoma, I know just how crucial early detection can be in saving lives.
My cancer journey has been an extensive and painful one, but it has also strengthened my resolve. It has inspired me to become an advocate for cancer patients, to educate others about the risks of hereditary cancers and to promote tools such as genetic testing that enable individuals to take control of their health before it’s too late.
When I was first diagnosed with colorectal cancer, I started to understand my family history and how genetics influenced my health. But it wasn’t until I tested positive for Lynch syndrome, a hereditary condition that greatly increases the risk of colorectal, endometrial and ovarian cancers, that I realized the extent of my predisposed risk. That diagnosis completely transformed my life, and I was forced to equip myself with the tools I needed to stay ahead of the disease. Now, I hope to do the same for others who might not be aware of their own risk.
While Lynch syndrome doesn’t guarantee a cancer diagnosis, it certainly increases the risk of one (or multiple, in my case). What it does guarantee is the need to stay proactive and vigilant about your health, something I think everyone, Lynch syndrome or not, should practice. We must take charge of our own health, empowering ourselves with information, discussing our health risks with our doctors, and staying up to date on recommended checkups and tests, including routine cancer screenings.
The deadliest cancers in Illinois are those of the lung, colon/rectum and prostate. These three cancers account for over half of all cancer deaths across our Prairie State. The good news is that these cancers also all have preventative screening tests available that can find cancer before any symptoms arise and treat pre-cancers and cancers early, before they have a chance to spread.
Having battled against and survived colorectal cancer, or CRC, I can attest to just how vicious it can be. But despite its high mortality, early-stage CRC has a remarkable five-year survival rate of 91%. And for endometrial cancer, the survival rate is 81%, increasing to 95% when the cancer is detected before it spreads beyond the uterus. These numbers highlight just how transformative regular screening and early detection can be.
Cancer screening technology has also come a long way in the past few decades, with innovative advances such as 3D mammography and low-dose CT scans for lung cancer. One of the most significant developments in cancer detection has been the emergence of noninvasive, blood-based tests that eliminate the perceived inconvenience and discomfort of some traditional screening methods.
Recently, the Food and Drug Administration approved the Shield test, the first Medicare-covered blood test approved as a primary screening for CRC. While genetic testing can identify those of us at higher risk for developing cancer, tools such as the Shield test offer an easier and less invasive option for early detection of CRC among average-risk individuals, representing an encouraging step forward in increasing accessibility for millions who might otherwise go unscreened. The test is also now covered for fellow veterans receiving community care benefits authorized by the U.S. Department of Veterans Affairs.
It’s important to note that tools like the Shield test don’t replace other screening methods such as colonoscopies or stool-based tests, or genetic testing for individuals with hereditary risks, and they are not intended for those who have Lynch syndrome and are high-risk.
But they are valuable additions to a broader tool kit in protecting our public health and a way to improve the early detection of CRC and hopefully save lives. If such tools had been available to my grandfather and brother, both of whom tragically lost their lives to CRC at ages 38 and 47, respectively, there is a very real possibility they could still be here today. Early detection through screening is often the difference between life and death, and without access to these lifesaving methods, their cancers went undetected until it was too late.
My advocacy has always focused on empowering patients to become their own best health advocates. When we understand our risks through family history and genetic testing, we can access earlier interventions and make better decisions for ourselves.
Cancer doesn’t wait, and neither should we.
_____
Wenora Johnson is a three-time cancer survivor and a Navy veteran who lives in the Chicago area.
_____
©2025 Chicago Tribune. Visit at chicagotribune.com. Distributed by Tribune Content Agency, LLC.


















































Comments