Vaccine situation will be complicated this year, experts warn
Published in News & Features
The ongoing drama in Washington over changes to national vaccine policy has many people wondering just how difficult and expensive it will be to get flu and coronavirus shots this fall. While experts say that the situation is still uncertain, the biggest changes are likely to impact healthy adults under age 65 who are covered by Medicaid, called Medi-Cal in California, the federal health coverage of last resort for more than 70 million Americans, nearly 1 million of whom live in San Diego County.
Those who are covered by private health insurance plans from their employers or purchased through health insurance exchanges such as Covered California are likely to see significantly fewer impacts, because most carriers have signaled that they intend to continue providing their members with COVID-19 vaccines at no additional cost, even if anticipated changes at the federal level end up removing their obligation to do so under the Affordable Care Act of 2010.
“Vaccination continues to be one of the safest and most effective ways to protect against illness and reduces the severity of your illness if you do get sick,” Kaiser Permanente said in a statement. “Vaccinations mean fewer sick days, hospital stays, emergency room visits and other health complications.
“As part of our commitment to preventive care, Kaiser Permanente will continue to offer no-cost coverage for flu, COVID-19, and RSV vaccines to our members. This aligns with the latest evidence as well as the actions of other leading health care organizations across the country, including AHIP and the American Medical Association.”
Indeed, AHIP, a trade group that represents American health insurance companies, issued a statement on June 24 indicating that its members “are committed to ongoing coverage of vaccines to ensure access and affordability for this respiratory virus season.”
But the situation is much less certain for Medi-Cal enrollees.
The California Department of Health Care Services, which runs Medi-Cal, confirmed in an email last week that children and young adults are in the clear because the state’s vaccination rules are different from those that govern adults.
“Under the federally mandated Early and Periodic Screening, Diagnosis and Treatment benefit, Medi-Cal covers a comprehensive set of services for Medi-Cal members under age 21, which would include any additional immunizations and vaccines (including COVID-19 and flu vaccines) that a Medi-Cal provider determines are medically necessary,” the DHCS statement said.
But the state agency could not say the same for those older than 21. If anticipated changes to the nation’s COVID vaccination recommendations were to occur, DHCS said it “would evaluate them and, if necessary, make updates or refinements to Medi-Cal policy.”
Medi-Cal does allow beneficiaries to file “treatment authorization” requests if they need a service that the program does not provide, but individual requests on the scale required for COVID vaccines would seem unworkable.
The agency did not provide additional information Friday on what those refinements might entail, but Dorit Reiss, a professor of law at UC San Francisco, whose vaccine policy research is widely cited, said that Medi-Cal, as a government program, has less flexibility than private health insurance companies. While there is an alternative to spend state funds in order to cover vaccination costs for Medi-Cal recipients, such a move would require further action.
The retail costs of existing COVID shots range from $137 to $141 per dose, according to the CDC.
“People who have (private coverage like) Kaiser, for example, are probably going to be able to get the vaccine fairly easily,” said Reiss said. “People who don’t are going to have a lot more issues.
“One thing that we’re going to see is unequal access.”
DHCS confirmed by email late Saturday afternoon that there is a “treatment authorization” process that can be used when a Medi-Cal patient has a medical necessity for care that the program does not cover; however, filing individual appeals for vaccination would seem to be difficult.
“If there are any changes to CDC/ACIP or other federal policy guidelines, DHCS will evaluate them and make updates or refinements to Medi-Cal policy if/as needed, to further clarify coverage,” the DHCS statement said.
Why this is the case comes down to the nation’s vaccine approval process.
Because respiratory viruses change rapidly, vaccines are updated annually, with virologists and epidemiologists determining which strains are most likely to be prevalent in the coming year and approving new formulations tailored to better match what’s likely to be going around in the coming fall and winter months when influenza and coronavirus spread most rapidly.
The key detail is that the U.S. Centers for Disease Control and Prevention, and a special expert panel called the Advisory Committee on Immunization Practices, reviews recommendations from the U.S. Food and Drug Administration to determine who should be vaccinated.
In the past, recommendations for coronavirus vaccines have been made for all Americans age 6 months and older. But this year, FDA officials have hinted that they wish to approve updated COVID vaccines only for Americans age 65 and older or who have medical conditions that put them at significantly increased risk of severe illness if they become infected.
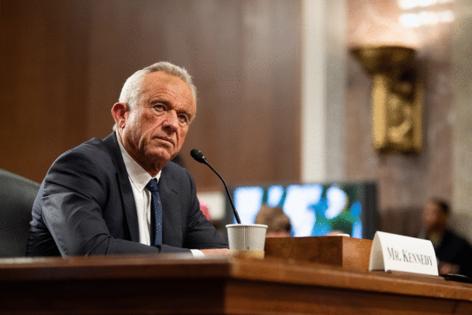
If the CDC and its ACIP advisory panel, which was recently upended by U.S. Health and Human Services Secretary Robert F. Kennedy Jr., ultimately approves a narrower recommendation for adult COVID vaccination, it will change the obligations of America’s private health plans under the Affordable Care Act. That federal law, often called Obamacare, mandates that insurers cover all routine vaccinations recommended by ACIP and the CDC at no additional cost.
But private insurance companies are free to continue covering them, even without a requirement to do so. And, with most professional medical associations and societies stating that they support sticking with broader inoculation schedules, those with health insurance are likely to be able to get shots this fall. Doing so, though, may be more inconvenient than it has been in the past.
This has already been the case for children and pregnant women. Though Kennedy removed the government’s COVID vaccination recommendation for these two groups from the CDC’s formal vaccination schedules in late May, medical providers have continued vaccinating these groups, working under recommendations from professional organizations such as the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists.
In addition, Medi-Cal and Medicaid programs have a tougher time providing medications to their beneficiaries “off-label” a term used to describe situations when drugs are prescribed to patients not listed in the FDA’s official documentation.
And there is also some variability in the legal protection that medical practitioners have when prescribing off-label, which would be the case if the CDC recommendation for COVID vaccines does not cover healthy adults younger than age 65.
Licensed physicians, Reiss said, have strong protections against lawsuits when they prescribe medications off-label, but pharmacists do not enjoy the same legal shielding. This means that if the government’s senior-focused recommendation comes to pass, pharmacies, often key locations for those without other medical coverage, may be unwilling to give updated COVID shots this season.
“People who need to get the vaccine from a pharmacist, or who have less comprehensive health insurance, or who depend on the federal health insurance system, are going to have more trouble getting vaccinated,” Reiss said.
It is not clear how the nation’s large drugstore chains will handle this wrinkle should the CDC’s vaccination recommendation for adults change. CVS Pharmacies said this week that it is reserving comment until action is taken.
“We won’t have more to share until the updated vaccine is authorized and we are able to review the FDA’s guidelines,” CVS said in an email.
Some, like Dr. John Bradley, an infectious disease specialist at Rady Children’s Hospital in San Diego, are concerned that any reduction in vaccine availability will hit those with the least means hardest, not just due to access, but also due to pervasive socioeconomic factors.
“Especially in lower-income families, there are often socioeconomic situations where there is more crowding in homes and the spread of viruses is easier,” Bradley said. “It means that children living in crowded situations are at greater risk of disease, and they are often in families that can least afford to pay out-of-pocket.
“In the past, they haven’t needed to pay out-of-pocket, because society believes that preventing a child from getting infected has major societal benefits in preventing that child from spreading it to others in the family and at day care, kindergarten and school, so it has been deemed worth it and that policy has been pretty effective.”
Some may wonder, given delays in giving final approval to a reformulated flu vaccine and to even more delayed COVID vaccine approvals, whether there will be enough supply on shelves this fall.
Even though final approvals have not yet been made, manufacturers say they are confident they can deliver. Moderna, manufacturer of one of two main mRNA COVID vaccines, noted that it did not receive final approval from the CDC until Aug. 22 of 2024.
“It did not impact our ability to produce ample supply for the fall season,” Moderna’s statement said.
Pfizer, which makes the nation’s other main mRNA vaccine, was equally confident that it could have an updated product on shelves quickly.
“Upon approval, we will begin shipping immediately and expect supply will meet demand through this season,” Pfizer said.
_____
©2025 The San Diego Union-Tribune. Visit sandiegouniontribune.com. Distributed by Tribune Content Agency, LLC.







Comments